Interoperability & Data Sharing: Roles in Behavioral Care Coordination
by Mike Lardieri, LCSW on November 21, 2022

In a recent white paper, Next Frontier of Care Delivery in Behavioral Health, I discussed a McKinsey & Co. report that identified 10 transformative ways care delivery will evolve over the next few years and how these 10 ways apply specifically — and significantly — to behavioral health. Now, in this column, I want to examine two of the topics covered in that white paper more closely: interoperability and data sharing. I will do so with a focus on the role these increasingly critical capabilities play in supporting and achieving better care coordination within and outside of behavioral health.
Current State of Interoperability and Data Sharing
Ever since the enacting of the Health Information Technology for Economic and Clinical Health (HITECH) Act in 2009, the healthcare system, and behavioral health within it, have been moving towards greater interoperability and data sharing. The reason is so that we can achieve better care coordination across the continuum of care.
Unfortunately, in today's healthcare environment, there remain too many instances when one or more healthcare professionals engaged with a patient lack the patient's current information at the point of care and are not fully aware of the different care and treatments the patient is receiving. It may happen less now than in the past, but even individual instances of failed interoperability and data sharing can have serious consequences for a patient.
Consider two providers unknowingly providing different medications that have contraindications. Consider one provider unknowingly providing a treatment that can cause complications with another provider's treatment. Consider lab results that come in and should influence treatment decisions, yet those results are not effectively shared across the continuum.
When there is a lack of interoperability and data sharing, we see serious inefficiencies in care. When people do not receive good care, they have bad outcomes. Bad outcomes lead to higher costs. It doesn't take much of a breakdown in interoperability and data sharing to lead to potentially significant problems for patients.
EHR's Effect on Patient Encounters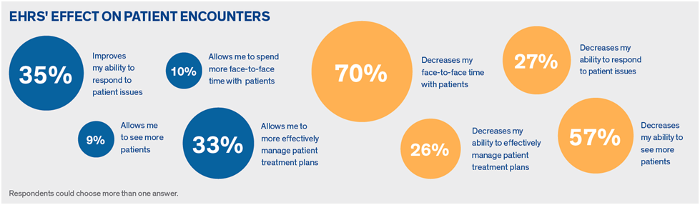 2017, Healthcare IT Today Deriving ROI from Data-driven EMR Clinical Optimization
2017, Healthcare IT Today Deriving ROI from Data-driven EMR Clinical Optimization
Work on creating a "unified community record" for patients is not new. Efforts were underway even before the large-scale adaptation of electronic health records. Yet creating such a record continues to elude us. We're still trying to get to the place where every provider knows what's going on with the patient, can see what's going on with the patient, can add their input to the treatment plan, and can communicate with the care team and with the patient, all while the patient has the full care team servicing and supporting them in person and/or virtually.
Addressing Social Determinants of Health
The care team is an important concept. In the past, a patient's care team was their doctors and nurses in a clinic. That's no longer the case. We now recognize the implications of social determinants of health (SDoH) and disparities in care and the ways in which these unresolved issues affect care. Some people are not able to access care appropriately because their SDoH issues get in the way.
Consider a person with housing insecurity. They may not spend the money to pick up their medication if they're worried about whether they can afford to keep their apartment. We see the same issues with food insecurity. Some people struggle to afford food and are being forced to make choices: Do I buy medicine for my kids, or do I buy food?
The challenges associated with SDoH and care disparities are familiar subjects for many behavioral health providers. What is new are the efforts of companies, including Core Solutions, to get behavioral health and other technology up to speed to support patients in ways that go beyond in-person care and take factors such as SDoH into consideration.
Interoperability greatly helps with this concept of, "whole-person care coordination." When we speak of interoperability in this context, it must be interoperability that extends across multiple provider types and non-provider types. As an example of the latter, consider a patient who receives assistance with receiving and completing a Supplemental Nutrition Assistance Program (SNAP) application. The person providing help to the patient should be a part of that patient's care team, and the information about the SNAP application should be known to the other members of the care team. Understanding that the patient is receiving assistance will help them cut food expenses. Other care team members will know the patient is in a better position to afford their medications and can emphasize the importance of making medications a high priority now that purchasing food is less of a financial burden.
The same logic applies to patients receiving assistance with housing and other services. There are care management organizations working to help patients get the services they need or may already have access to, such as through Medicaid, Medicare, or other benefits. Many patients are unable to find or complete the documentation required to access those benefits. When they receive help, the individual providing the assistance becomes part of the care team.
The Relationship between Care Management and Care Coordination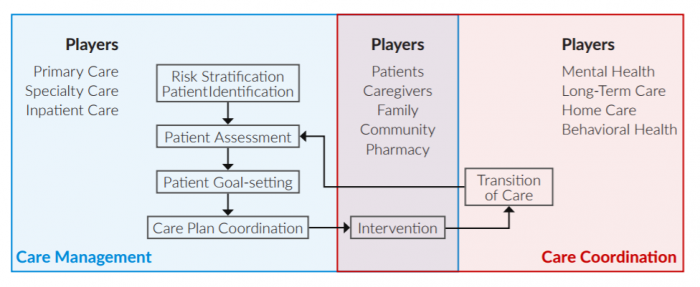 2017, Chillmark Research
2017, Chillmark Research
Achieving and maintaining whole care coordination is essentially impossible without technology. You require a platform that can accommodate multiple people sharing information about the patient, with the patient's consent, when necessary. For HIPAA providers, sharing information is covered under HIPAA. For non-HIPAA providers, you need consent from the patient. As long as you have that consent, technology must permit providers to add people from outside the care team to the team. It then must take those people in and out at the patient's request or once an activity is completed and an individual or organization no longer needs to be involved in the care coordination process.
Attaining this level of functionality is not easy, but it is imperative if we want to provide the level of whole-person care coordination that can help deliver better outcomes for our patients. That's why we've made achieving such functionality a priority at Core. We're proud that our Cx360 platform effectively supports inviting other providers to participate in the patient's care plan and provides the documentation that helps keep everyone on the same page and working toward the same health goals.
Interoperability for Patient Communication
The value of interoperability extends beyond internal communications between care team members. Improved interoperability translates to improved sharing of information and communication with patients.
A significant facet of the 21st Century Cures Act concerns patients having access to their own data and in a format that permits ease of moving their data around. Access to data helps patients be more engaged in their treatment, and we know those who are more engaged in their treatment typically achieve better outcomes because they're paying closer attention to their care. The ability to move data helps ensure patient care is not disrupted when patients travel, relocate, change providers, or add new providers.
Other forms of interoperability, including secure messaging between providers and patients, further demonstrate the importance of implementing a technology platform that prioritizes interoperability.
Importance and Shortcomings of Data Sharing
The reason you want to prioritize interoperability is for data sharing. There are specific constructs for how behavioral health providers share data. The problem in the field right now is there are still some nuances to these constructs which lead to different interpretations of how the data should flow. That then contributes to difficulties with sharing data. In some instances, the obstacle that must be overcome is an interoperability variability between two groups preventing data from seamlessly flowing from one group to another. The groups must then identify where they can establish a link so they can view the data the same way.
There's a specific set of data we use in the United States called USCDI (United States Core Data for Interoperability). It provides all the fields we're currently using for data sharing. USCDI has a method to share data through different vehicles. If you want to share a consult note, there's a certain set of data you send for a consult note. If you want to share a discharge summary, there's another set of data using different data elements from this master set for the discharge summary. Then there's a comprehensive care record, also referred to as a CCDA or consolidated clinical document architecture, which takes all the data fields, packages it up, and sends it along.
USCDI Example Fields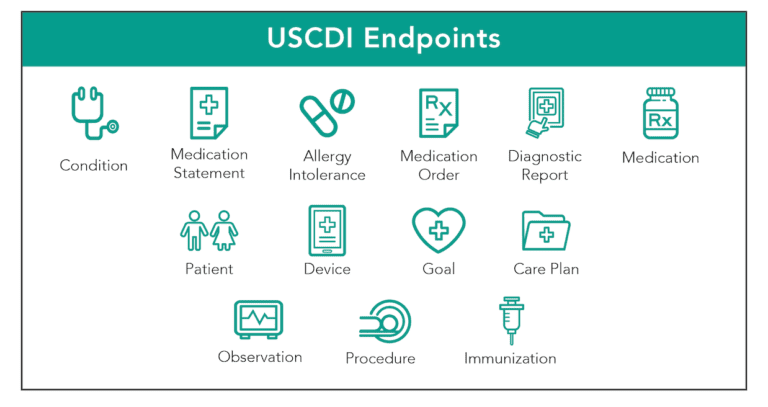 2019, Datica
2019, Datica
On the one hand, it's terrific that we have the constructs for sending the data. But what's important around that is organizations must be able to segment their data and send only specific sections of the data when it's necessary. What do I mean by segmented? Consider the paradigm of a paper chart. We had a tab for labs, a tab for medications, a tab for treatment plans, etc. It's that same kind of construct. The patient or provider should be able to choose what segment of data — i.e., tab — to send to another provider. You don't necessarily need or want to send everything in the record every time. You may just want to send those sections that were updated to the other provider, which means you must be able to select from labs, medications, progress, notes, history and physicals, etc.
Within the Core Cx360 platform, we offer about 15 different segments that providers and patients can choose from. Using Core's process, the provider or patient can send the CCDA or choose which segments of data they want to send to the next provider. That's a very powerful functionality. It saves time in care coordination because now the receiving provider does not need to wade through everything to determine what's new and changed. Instead, they're just going to be reviewing the updated information.
Value for Substance Use Services
The ability to segment data is extremely important for any provider delivering substance use services. Consider that 42 CFR Part 2 — "Confidentiality of Substance Use Disorder Patient Records" — requires a slightly higher level of confidentiality than HIPAA. It essentially requires providers to segment their data for data-sharing purposes. Substance use disorder patients are expected to have the capability to request that providers only share some data and not their full records.
If a patient wants to segment their data but the technology used by the SUDs provider can't do so, now the patient doesn't have such an option. They must send all their data if they are going to share any data. They may decide that rather than share all their data, they won't share any, so no data moves between providers.
At Core, we've made complying with 42 CFR Part 2 a priority. Our platform supports this data segmentation, thus meeting patient, provider, and regulatory needs.
HIE Implications
Such segmented data-sharing capability is also very important for sending information to health information exchanges (HIEs), which we recognize is critical to strengthening whole-person care coordination. At Core, we've built our workflow designer to support more seamless data sharing with HIEs. The workflow designer can be set up so that action automatically occurs based on the return of a result. For example, if a new lab result comes in, then that new result — and only that new result — can be automatically sent to the HIE to update the master HIE record, which is where all providers are now looking to receive information from or about the patient.
At the moment, there are a lot of one-on-one exchanges going on between providers and individual HIEs, and that will likely continue for a while. But efforts are underway to push everything through local, regional, and national HIE structures. The idea here is that each provider will send its updates to the HIEs. When a patient visits another provider, the provider queries the HIE. If the patient has been treated by multiple providers, that information will be available through the HIE, and the new provider will be able to consume that information. Within seconds, the new provider can receive a good view of what has happened to their new patient over time.
A challenge we're encountering is that the information available through HIEs is limited to the data that came into the HIEs. When providers fail to send data to HIEs, now we start to have gaps in the patient record. Small gaps can be significant for the reasons noted earlier. Data sharing with HIEs are still not perfect. While nearly all hospitals are sending data to HIEs, there's a much lower percentage of ambulatory providers connected to HIEs.
Health Information Exchange (HIE)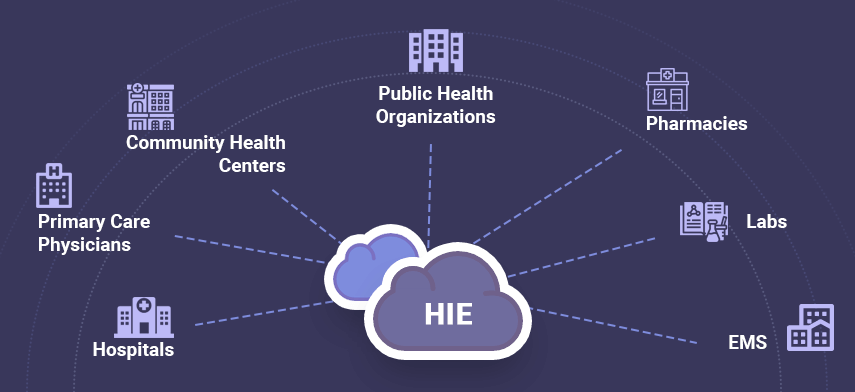 2019, Mobisoft
2019, Mobisoft
On the ambulatory provider side, we're not just discussing medical providers. Ambulatory providers include physical therapists, and occupational therapists — essentially everybody who touches the patient when they leave a hospital or are involved with them on an ambulatory basis. Consider a patient who undergoes hip surgery. They are going to require treatment from multiple people for their recovery, but it's likely that not all those treatment providers will be connected to the HIEs.
Data uncertainty is also a problem on the receiving side with providers. Providers want to trust the systems they use. They should know if they are receiving a portion of a section of data, a complete section, or an entire patient record. Currently, what is and isn't being shared is not always clear.
It's my personal opinion that we should inform providers if a record goes to them and pieces are omitted. We know patients don't tell providers everything anyway, and providers must always check what they receive from the patient. Patient information cannot be automatically consumed blindly. But the more information that is shared, and knowing more details about the information that's included, can only help with strengthening care coordination.
National Progress
That's the lay of the land today. Things are improving, but they need work. The good news is that there are a few projects underway focused on improving data sharing across the country. This includes The Sequoia Project.
There are also a few consortiums, including Carequality, CommonWell Health Alliance, and eHealth Exchange, that have brought large hospital systems together and now have frameworks and contracts that bind participants to a common agreement that fosters trust in the sender and the data. That's all being worked on now, and it's having great success. We're just not at 100% of the country yet, but we're getting there.
Interoperability and Data Sharing: Key Takeaways for Behavioral Health Providers
Interoperability and data sharing is no longer wish list items. If you're a player in healthcare — whether you're a medical provider, behavioral health provider, care management organization, or other SDoH organization — you're going to need to have a vehicle to achieve interoperability and data sharing. We know and are sympathetic to the fact that some SDoH organizations are strapped for finances. These organizations must look for partners that can provide the technology to allow for highly efficient and cost-effective data sharing.
We advise organizations to make sure interoperability and data sharing are regular topics on their senior leadership meeting agendas. It may be easier to frame the discussion on interoperability and data sharing around electronic care coordination.
The next step for providers is to plan to add the technology to support these care coordination initiatives. First, look for systems that have the capabilities discussed in this column. By regulation, any platform that can achieve these capabilities must be ONC certified, but they all function a little differently. Look at the platforms and have their vendors walk you through how they support data sharing. Review what the process looks like and how the organization completes it within the platform. There are easy ways and hard ways to do it.
Finally, reach out to your local HIE. You can view a list of the current HIEs on the local level and the state level. Some states have multiple HIEs, while others just have one. They're all very helpful because they want providers to participate. Tap into their knowledge and begin to move your organization forward.
- Behavioral Health (38)
- EHR (22)
- AI in Healthcare (17)
- I/DD (16)
- Mental Health (14)
- Revenue Cycle Management (12)
- CCBHC (11)
- Electronic Health Records (9)
- Crisis Center (8)
- COVID-19 (4)
- Substance Abuse (3)
- Augmented Intelligence (2)
- Care Coordination (2)
- Addiction Treatment Software (1)
- Billing (1)
- Checklist (1)
- Substance Use (1)
- Telebehavioral Health (1)


