Examining the Future of Augmented Intelligence for Behavioral Health
by Ravi Ganesan on January 21, 2025

There’s no denying that artificial intelligence (AI) is becoming instrumental to improving behavioral health operations and care delivery. As organizations struggle with the ongoing staffing crisis and the complexities of designing effective, personalized treatment plans, AI holds a world of promise we’re only beginning to understand. That said, our responsibility as leaders is learning not only the benefits of AI but also how to adapt to its limits while safely developing and adopting new tools.
Becoming a provider of responsible AI is critically important to the team at Core Solutions. We believe that a measured approach to artificial intelligence — one that prioritizes augmented intelligence for behavioral health over fully automated AI — will benefit all parties in the coming years. Let’s examine why, as well as what this means in practice and for the foundation of Core’s product roadmap.
How Mental Health AI Can Help Tackle Provider Challenges
Over one-third of the U.S. population lives in a mental health provider shortage area, according to the National Center for Health Workforce Analysis, with rural residents and Medicare and Medicaid enrollees disproportionately impacted. As the number of people with mental health conditions and substance use disorders has risen nationally in recent years, clinicians and staff have felt the strain of burnout as clients either wait extended periods for care or go without professional help. Technology advances like AI have been vital in supporting a return to clinical excellence, yet many practices remain hesitant about adding AI because of a variety of factors, from cost to integration concerns to clinician reluctance, fear, and lack of digital skills.
However, when clinicians can retain control over clinical decision-making while receiving assistance from technology — otherwise known as augmented intelligence for behavioral health— they get the most benefit from mental health AI tools. Whether by supporting streamlined documentation, client diagnosis, or recommendations for evidence-based practices, this form of AI in mental health facilities saves time and creates efficiencies that give providers back crucial minutes for direct client care while reducing administrative burden and contributing to improved job satisfaction.
Our Method for Developing Augmented Intelligence for Behavioral Health
In the context of healthcare, and particularly behavioral health, AI is not designed to replace the clinician’s judgment. There are too many intricacies involved in understanding and diagnosing clients, so in most cases, AI in mental health needs a human touch. For example, Core has a chatbot that can answer questions about data in our system, but it’s not intended to communicate with people about their condition or with empathy or nuanced interaction that could lead to inaccurate or biased recommendations.
This is not to say that fully automated AI cannot have some measure of autonomy, however, and it is useful for noncritical clinical work and bridging knowledge gaps. For example, as organizations hire new staff and less experienced providers, AI can complete tasks that these individuals initially lack the experience to do on their own.
These factors are, in part, why we want to educate customers on how augmented intelligence for behavioral health works and how to successfully implement it as we develop new solutions. There is still risk involved with the adoption of augmented intelligence, and an understandable reservation over how it’s trained and whether the type of data used will introduce unfair biases, inaccuracies, or hallucinations. We have placed a priority on being fully transparent about the models we utilize so that, by the time pilot projects are launched, they aren’t met by frustrated customers and followed by a return to the drawing board.
Developing mental health AI products is an iterative process that may take several steps before you know you’re charting the right course and multiple iterations before you reach a finished solution. Core takes care to pinpoint specific use cases so that strategic planning and algorithm training is targeted around a meaningful answer to a clear problem, whether it's burnout, misdiagnosis/underdiagnosis, compliance challenges, or another pressing issue. More than anything else, we understand the importance of data and the need to collaborate with all stakeholders to ensure we get our solutions right.
Mental Health in AI: Solutions to Empower Providers and Boost Care
As AI matures over the next few years, we believe that augmented intelligence for behavioral health can and should be at the forefront of elevating everything providers do. This includes supporting better communication with clients, enhancing diagnostic acumen, and promoting more effective care coordination and plans. This, in turn, gives clients greater access to superior service, empowers their participation in their care journey, and creates balance in the care equation that adds up to happier, healthier stakeholders on both sides. It’s why our current and future product plans are rooted in use cases that position providers to focus on doing what they do best — caring for clients — and helping them do it better.
Ambient listening (a.k.a. ambient documentation), a technology that uses AI to record and transcribe conversations between a clinician and client and then generate notes, is a simple yet powerful tool that saves providers the monotonous work of capturing their thoughts during and following a clinical session. Ambient listening also enables providers to be more present during a session, thus building stronger client relationships founded on attentiveness and trust. Because of this technology, providers are able to pay more attention to what they may be intentionally or unintentionally expressing with nonverbal communication, which accounts for a staggering 60% to 90% of total communication, and practice deep listening, which has been found to be effective in engaging patients and better understanding their main concerns, and which ultimately contributes to better outcomes.
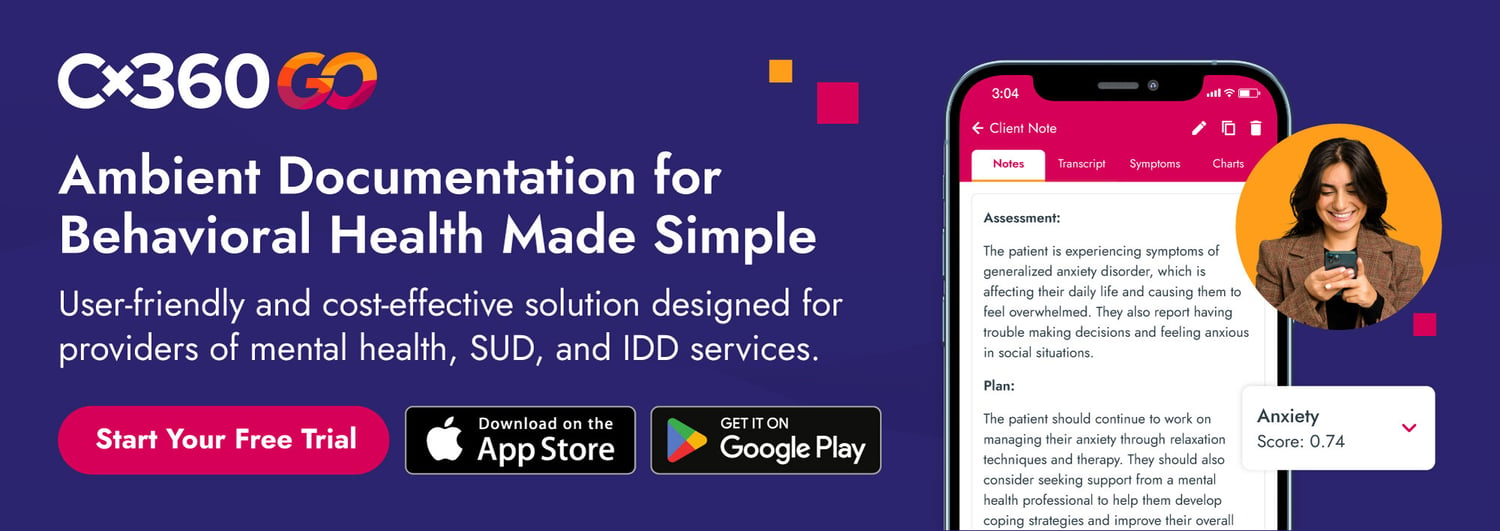
Core is placing ambient listening at the center of our new Cx360 GO app, which allows providers to conduct clinical sessions anywhere, securely transcribe conversations in a variety of formats with a single click, and upload those notes within seconds to the Cx360 EHR or any other system.
Since behavioral health conditions and AI in mental health practices are both multifaceted, Cx360 GO also analyzes those notes and, using ICD-10 codes, identifies symptoms and possible diagnoses in a simple chart that helps providers make connections they might not have otherwise considered. Clinicians can then use that data to create more personalized, accurate treatment plans with ideal evidence-based practices and track client history, including changes and trends that could signal the need for adjustments as treatment continues.
Architecting AI: The Role of Autonomy Amid Continuing Advances
In the near future, we'll see AI given more autonomy. On the nonclinical side of healthcare, we welcome innovations focused strictly on rules and data that are already on the horizon. We foresee, for example, that likely within just two years, most of or the entire revenue cycle management process will be fully automated, with the functionality for that shift available in 2025 and then a period of customer validation to follow.
Still, for clinical purposes, augmented intelligence for behavioral health will probably always be the AI of choice. We’re excited for some features in our upcoming products that will allow for a level of autonomy — such as the ability of Cx360 GO to provide feedback on notes and send them for review when necessary, or our scheduling software’s capability to weigh double appointment-booking when a client is identified as unlikely to show up — but a human will always make the final decisions.
As we share more knowledge about artificial intelligence and AI continues to amass a wealth of data, Core and other companies will develop even more use cases, features, and products that are sure to drive a brighter future for the behavioral healthcare industry, lifting up providers and improving measurement-based client care and outcomes. It’s critical that we never stop finding new paths forward.
- Behavioral Health (38)
- EHR (22)
- AI in Healthcare (17)
- I/DD (16)
- Mental Health (14)
- Revenue Cycle Management (12)
- CCBHC (11)
- Electronic Health Records (9)
- Crisis Center (8)
- COVID-19 (4)
- Addiction Treatment Software (3)
- Substance Abuse (3)
- Augmented Intelligence (2)
- Care Coordination (2)
- Billing (1)
- Checklist (1)
- Substance Use (1)
- Telebehavioral Health (1)